Case Study: Streamlining Provider Onboarding & Training for a Regional Health Plan
How a health plan accelerated provider onboarding and training while greatly reducing staff time and effort
In today's fast-paced managed care environment, timely and efficient provider onboarding is essential to
member access and regulatory compliance. A Western U.S.-based Medicare Advantage health plan serving
15,000 to 20,000 members partnered with Serious Development to modernize their fragmented onboarding and
training process. This intuitive web application reduced onboarding times by 50% and saved the health
plan's contracts and credentialing team hours of work daily.
PROJECT OVERVIEW
PROJECT DETAILS


Project Type
Custom Software Development
Technologies
CentralReach Integration
PROJECT SUMMARY
We built a centralized web-based Provider Onboarding and Training App designed for both external providers and internal health plan teams. It includes document submission, digital attestations, training module tracking, and real-time status updates—all integrated with the client's existing systems. The application improved the provider experience while aligning internal departments including Credentialing, Contracting, and Provider Services.


THE CLIENT
Situational Overview
Serious Development modernized the fragmented onboarding and training process for a Western U.S.-based Medicare Advantage health plan that serves 15,000 to 20,000 members. A centralized, web-based Provider Onboarding and Training App. streamlined the process for both external providers and internal health plan teams, offering features like document submission, digital attestations, training module tracking, and real-time status updates.

CHALLENGES
Overview



Manual onboarding process with back-and-forth emails and spreadsheets.
Lack of integration with provider portal and systems like EZ Cap and Wipro.
No real-time visibility into onboarding and training status for providers or internal teams.
DETAILS
- Existing tools couldn’t support digital attestations or training tracking.
- Providers had to download forms, sign manually, and email them back.
- Health plan staff had to manually verify document receipt and completion.
- Departments were siloed, and onboarding status was not visible across teams.
THE SOLUTION

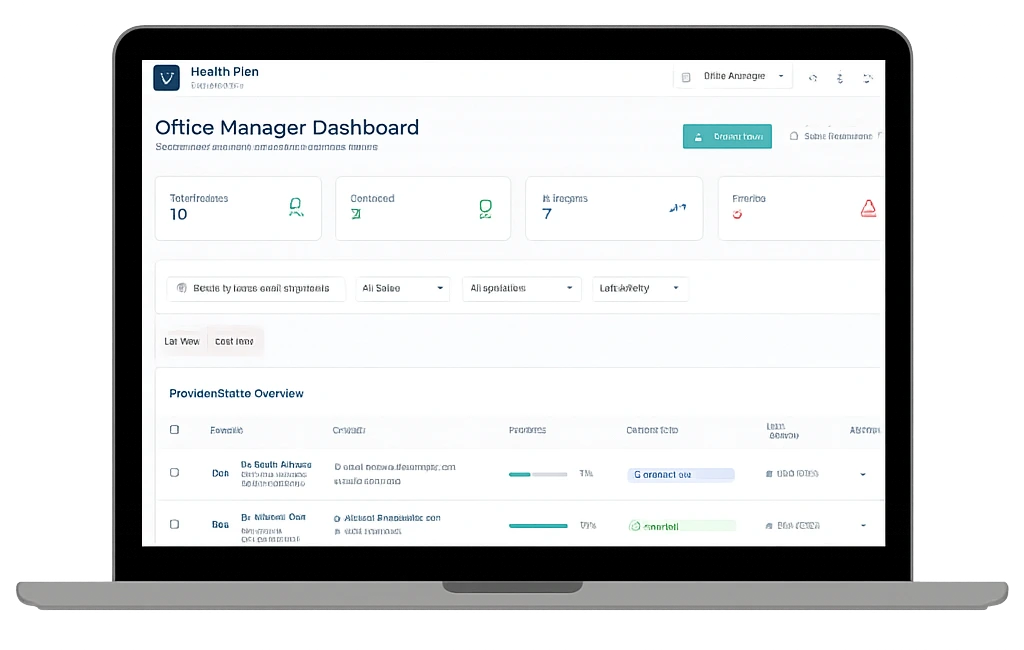
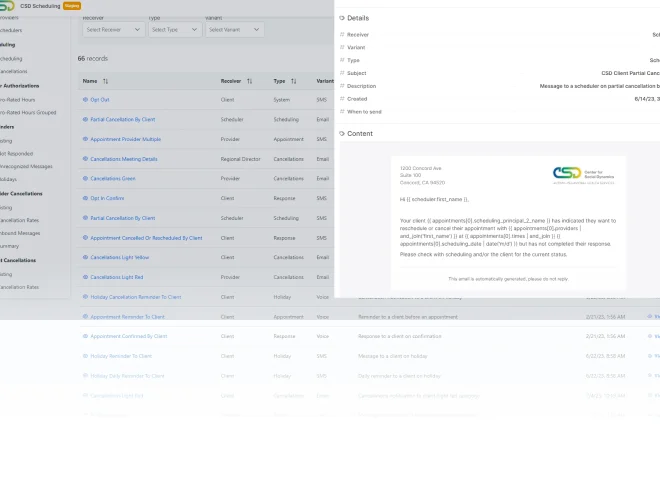
- Provider and Staff Dashboards: Providers and office managers could log in to view onboarding and training tasks.
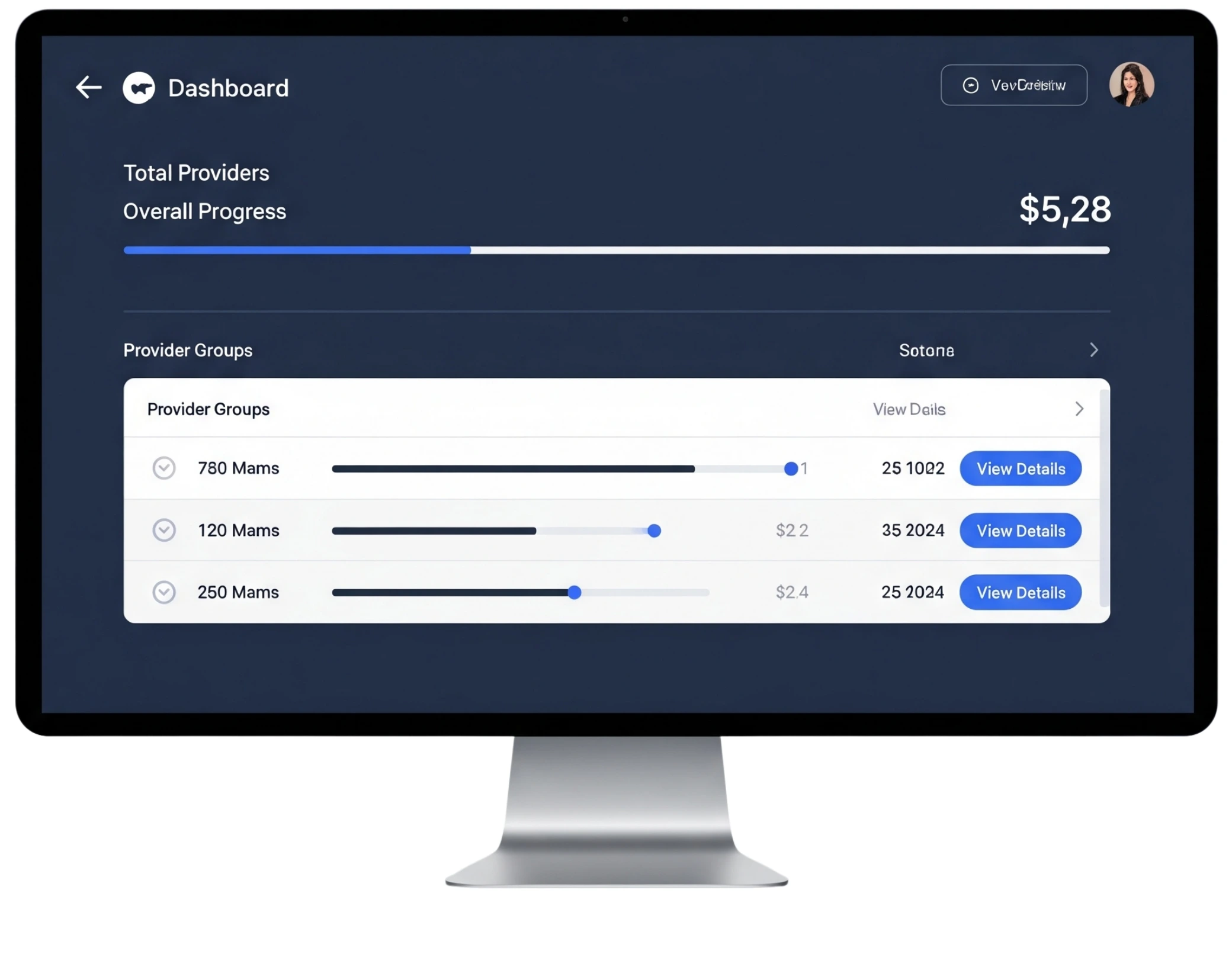
- Health Plan Dashboards: Internal health plan departments accessed a real-time dashboard for tracking progress, approvals, and document status.
- Training Module Completion Tracking: Providers completed required CPS modules within the app, tracked automatically and reported to internal systems.
- Custom Signature and Attestation Workflow: Attestations were signed within the app using our built-in signature feature, eliminating the need for printing, scanning, and emailing, and saving thousands of dollars annually vs using off-the-shelf software.
- System Integration: Bi-directional integration with EZ Cap and Wipro ensured that data flowed seamlessly between onboarding and backend systems.
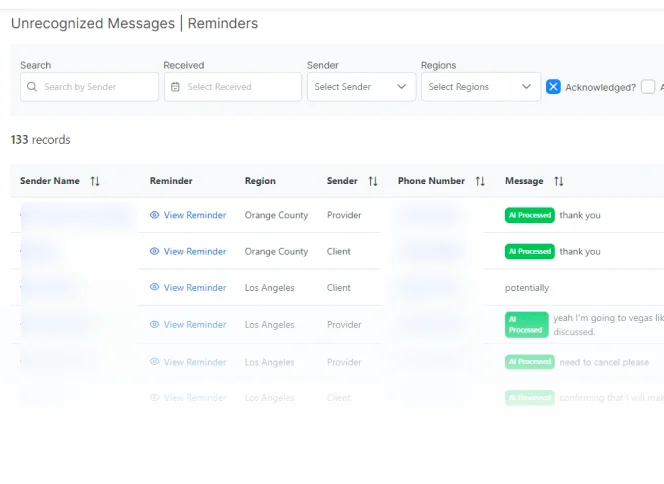
- AI-Driven Response Handling: Processed non-standard responses like “My child is sick so I need to cancel” by automatically confirming cancellations with empathetic and accurate responses.
- Role-Based Access and Self-Service: The system included two provider-side roles (provider and staff/office manager) and internal health plan roles (admin and super admin), with admins able to update training and attestation requirements annually


“This solution completely transformed how we engage with new providers. What used to take days now takes
minutes—and our teams finally have the visibility we needed.”
 Star Rating
Star Rating
Other Case Studies
AI-Powered SMS and Email Messaging App
Client and Employee Scheduling App for ABA
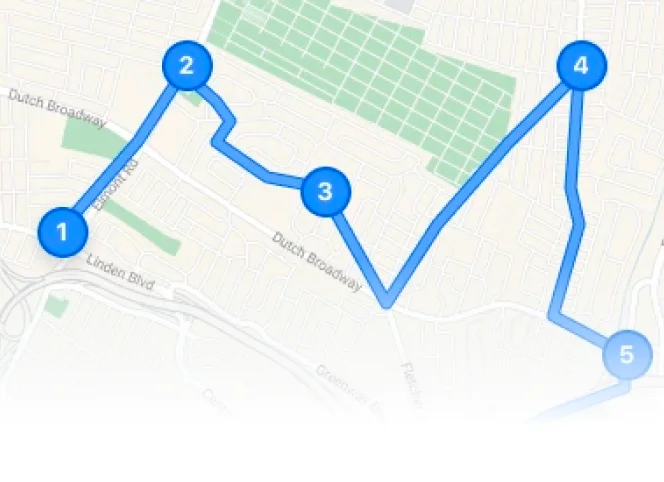
Scheduling and Map Routing App for Medical Clinic