Case Study: Streamlining Member Experience & Reducing Support Costs through a Custom Member Portal
How a Custom Portal Helped a Regional Health Plan Cut Support Volume by 70% and Boost Member Satisfaction
This case study shows how one regional Medicare Advantage plan serving 20,000–50,000 members transformed
its member experience with a custom-built portal. The result? A 70% drop in support volume, faster
service, and happier members.
PROJECT OVERVIEW
PROJECT DETAILS


Project Type
Custom Software Development
Technologies
EZ Cap Integration
PROJECT SUMMARY
Over a 4-month development cycle, Serious Development delivered a custom, HIPAA-compliant Member Portal for a multi-state health plan. Built on AWS and fully integrated with EZ-CAP, the portal gave members secure access to claims, benefits, ID cards, provider directories, and personalized plan messages. The goal was to reduce inbound support volume and improve member satisfaction through self-service. Post-launch results included a 70% drop in calls and emails and a 20-point increase in NPS—exceeding both operational and engagement targets.


THE CLIENT
Situational Overview
The health plan faced a growing volume of member support requests due to limited digital access to key information like benefits, claims, and provider networks. Members had to rely on live agents and email—often waiting days for responses—while staff spent hours re-entering contact updates and fielding repetitive inquiries. This not only strained internal resources but also negatively impacted member satisfaction and CMS Star Rating performance. The plan needed a scalable, self-service solution to modernize engagement and reduce operational burden.

CHALLENGES
Overview



High Support Volume & Operational Strain:
Members relied on phone calls and emails to access basic plan information—leading to long response times, staff overload, and manual errors in data entry.
Low Member Satisfaction & Engagement:
Without an intuitive digital experience, members were frustrated by delays, lack of transparency, and limited control over their health plan interactions.
Fragmented Systems & Manual Processes:
Critical member functions—like updating contact details, accessing ID cards, or checking claims—required multiple disconnected systems and manual staff involvement, reducing efficiency and accuracy.
THE SOLUTION
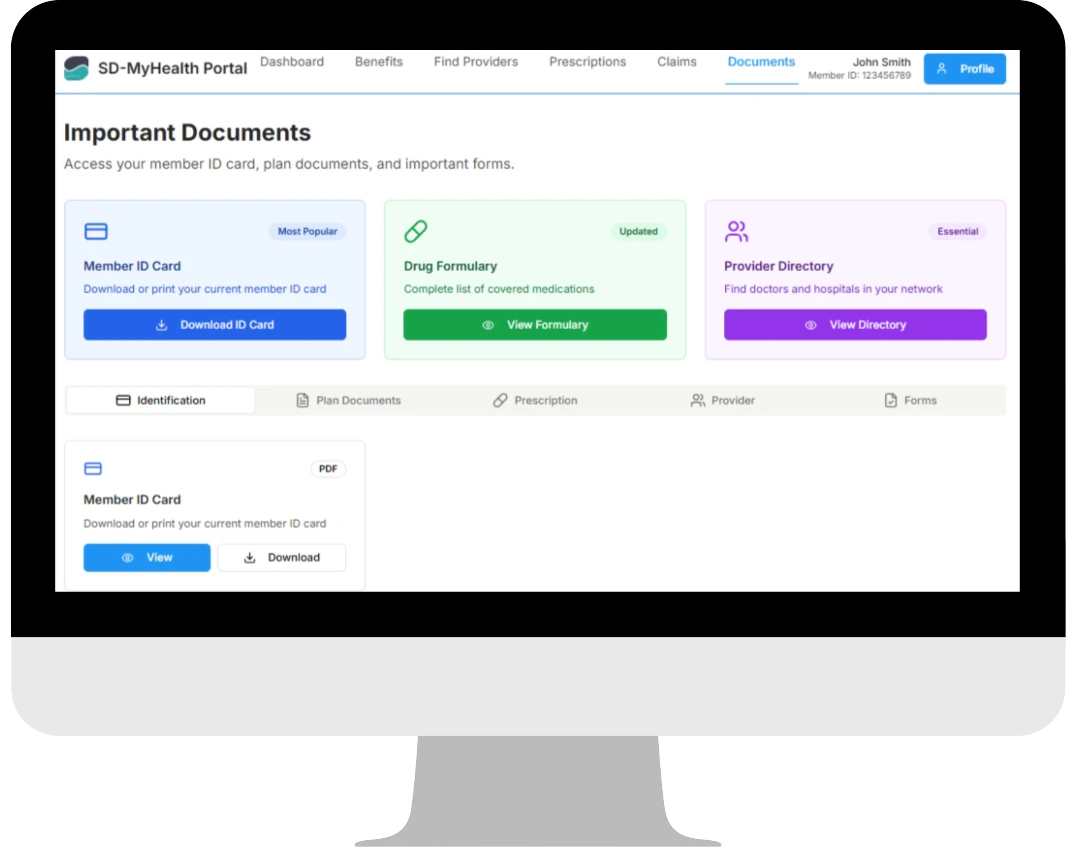
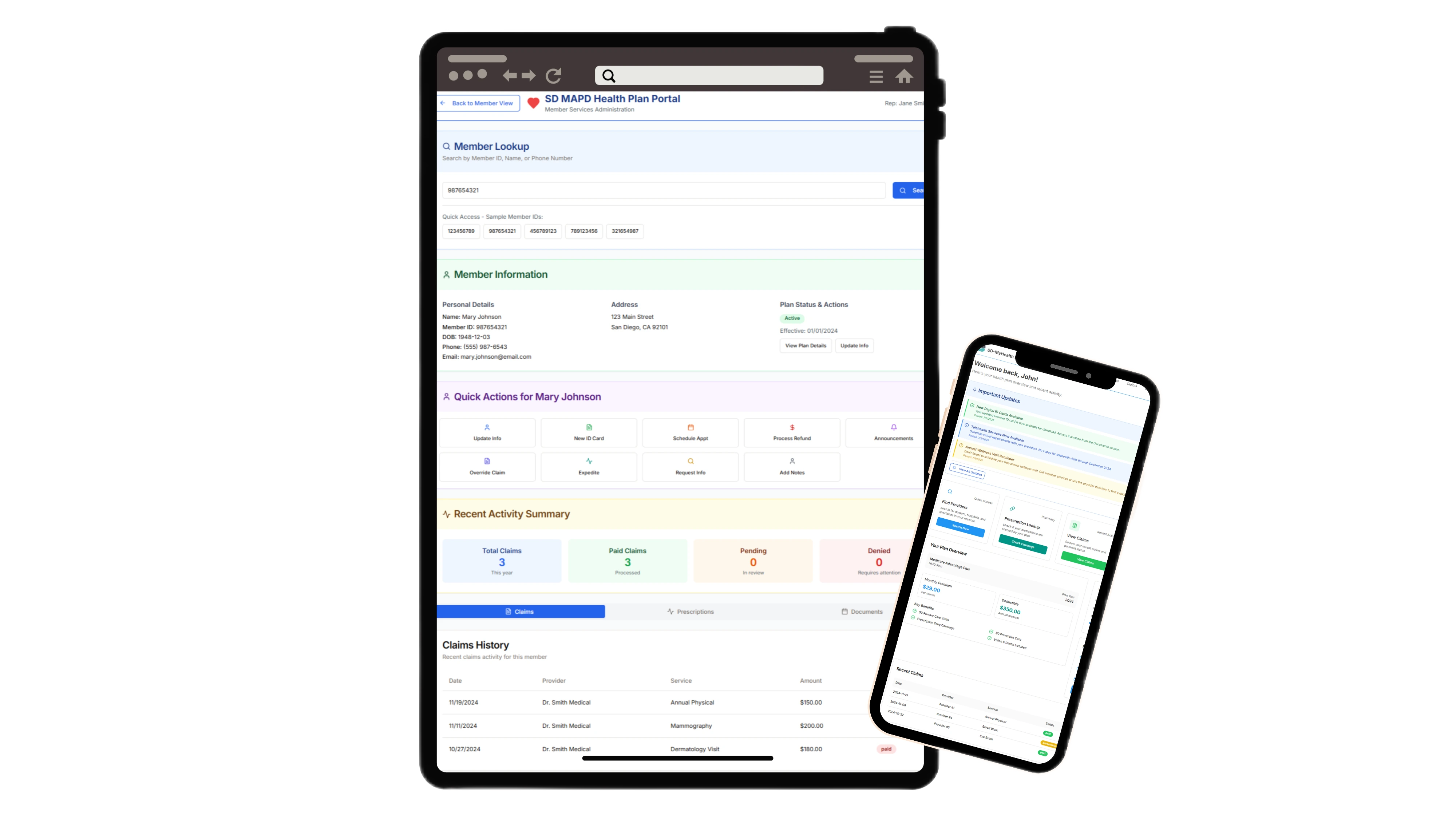 To address the fragmentation, support burden, and poor member experience, Serious Development designed and implemented a custom, HIPAA-compliant Member Portal. Built on AWS and fully integrated with EZ-CAP, the portal consolidated all core member services into a secure, user-friendly web interface. It enabled real-time access to claims, benefits, ID cards, provider directories, and messaging—while dramatically reducing the need for manual staff intervention.
Main Components Developed:
To address the fragmentation, support burden, and poor member experience, Serious Development designed and implemented a custom, HIPAA-compliant Member Portal. Built on AWS and fully integrated with EZ-CAP, the portal consolidated all core member services into a secure, user-friendly web interface. It enabled real-time access to claims, benefits, ID cards, provider directories, and messaging—while dramatically reducing the need for manual staff intervention.
Main Components Developed:
- Custom Web Portal (HIPAA-compliant) with secure login and role-based access
- Full EZ-CAP integration for real-time data on claims, authorizations, and eligibility
- Personalized member dashboards with health goals, plan documents, and messages
- Secure messaging system for plan announcements, renewals, and alerts
- Self-service tools to update address, phone, and email—no staff re-entry required
- Printable member ID cards and provider search with map/directions
- Back-office tools for Member Services to send targeted alerts and upload documents
Results
By replacing fragmented communication channels with a secure, fully integrated Member Portal, the health plan achieved measurable improvements in both operational efficiency and member satisfaction. The custom solution not only reduced inbound support volume by 70% but also empowered members with real-time access to their health data, benefits, and provider resources. With a scalable architecture and future-ready integrations, the portal now serves as a foundation for continued digital innovation across the organization.

“We needed a digital experience that made things easier for both our members and our team. This portal not
only reduced our support volume—it completely changed the way we engage with members.” - Executive Sponsor,
Medicare Advantage Plan
 Star Rating
Star Rating
Other Case Studies
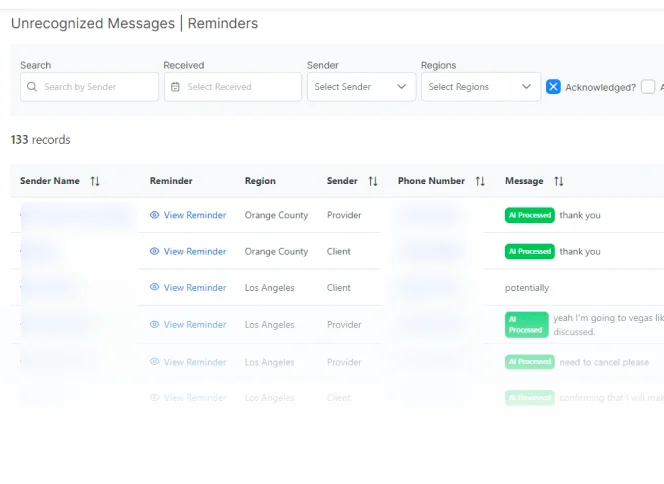
AI-Powered SMS and Email Messaging App
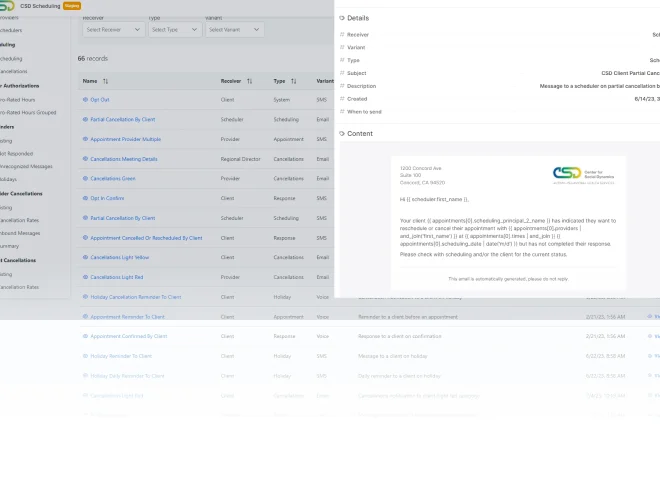
Client and Employee Scheduling App for ABA
Scheduling and Map Routing App for Medical Clinic